Wow Vision Therapy Blog
Harvard Research Shares New Info on Concussions & Vision

As parents, we want our children to engage in activities that will help them grow and develop confidence. The importance of extracurricular activities, such as sports is key in personal development and achievement. However, as in anything worth doing there can be risks involved. For the student-athletes engaged in physical sports ranging from soccer, football, hockey, and even competitive cheerleading, there is the chance of sustaining a concussion.
The American Medical Society for Sports Medicine position statement: concussion in sports states, “It is estimated that as many as 3.8 million concussions occur in the USA per year during competitive sports and recreational activities; however, as many as 50% of the concussions may go unreported.” Further, it states, “While the majority of concussions resolve within 7–10 days, in some cases symptoms persist for weeks, months or years beyond the initial injury.”

Those who suffer from chronic concussion-based symptoms, at the root of these symptoms are typically visual problems that, when left untreated, are tough to manage. From the words of one of our patients, “My journey started about 5 years ago when I had a pretty significant hit to my head. Shortly after that, I began to notice some negative changes in my vision. My eyes would become fatigued after the simplest of visual tasks. They felt like they were being pulled apart when reading anything up close, I had blurry vision, double vision, light sensitivity, and headaches. It got to the point where I would completely avoid using a computer, TV, etc. Even driving made my eyes symptomatic. It was a tough time for me to say the least.”
Indeed, persistent visual problems and related frustration are often in these patients with chronic concussion-based symptoms. Therefore, the first step should begin with a referral to a vision care provider for a comprehensive eye health and vision evaluation. Yet, while this might seem like the solution to the problem; if the doctor limits the evaluation to eye health and refraction for glasses alone, critical categories of visual function related to eye coordination involving binocular vision/vergence (eye teaming), accommodation (eye focusing) and oculomotor function (eye tracking) may be overlooked.
One crucial example of eye coordination involving binocular vision involves testing of the two eyes performing “convergence.” If the doctor does a procedure called the Near Point of Convergence Test, they will often find the patient with post-concussion symptoms to exhibit difficulty with convergence to an average ability (<7cm). As a result, they may diagnose the patient with Convergence Insufficiency.
However, as in anything complex, such as the visual complications associated with a concussion, the notion that performing a single test yields the complete diagnosis and single treatment are worthy of caution. To this point, new research by Harvard Medical School makes a clear case for a more comprehensive vision evaluation for those with chronic concussion-based symptoms. In their article, Post-Concussion: Receded Near Point of Convergence is Not Diagnostic of Convergence Insufficiency; the researchers conclude that not only post-concussion patients have a reduced near-point of convergence but, these patients have additional complicating visual diagnoses that we must address.
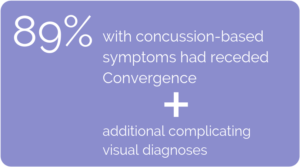
Their research found, of those with chronic concussion-based symptoms, 89% had a receded Near Point of Convergence. However, in addition, these same patients with a receded NPC had an array of oculomotor (eye tracking), accommodative (eye focusing) and binocular/vergence (eye teaming) dysfunction. Put another way; their reduced NPC was just the “tip of the iceberg”.
Specifically, of the 89% of those patients with a receded NPC:
- 95% had an oculomotor disorder
- 84% had deficits in accommodation (solely 41% or in combination with vergence disorders 43%)
- 54% had vergence disorders (also usually accompanied by an accommodative disorder 78%)
Whereas, convergence insufficiency “standing alone,” was found in only 6% of the cases
Therefore, their conclusion reads: “Because treatment options for the various oculomotor dysfunctions differ, it is prudent that these patients (with concussion-based symptoms) undergo a thorough examination of their vergence and accommodative systems so that an accurate diagnosis can be made and appropriate treatment prescribed.”
Appropriate treatment, as outlined by the American Optometric Association in the Clinical Practice Guideline (CPG-18) for Accommodative and Vergence Dysfunction, is office-based optometric vision therapy/rehabilitation.
For parents looking for answers when their child or student-athlete is experiencing chronic concussion-based symptoms; appropriate and effective treatment for these complex sensorimotor problems requires a comprehensive office-based vision rehabilitation model. This approach includes the integration of binocular/vergence function with accommodation and oculomotor function by a skilled vision therapist applying appropriate lenses, prisms and therapeutic tints prescribed and supervised by an experienced Doctor of Optometry who specializes in developmental vision and rehabilitation.
At Wow Vision Therapy, this is the focus of our entire team of Board Certified Doctors and Vision Therapists who provide the very best care available to remediate the complex visual problems associated with chronic concussion-based symptoms so our patients can quickly return to learn, return to work, return to play… and, Return to YOU!
 Dan L. Fortenbacher, O.D., FCOVD
Dan L. Fortenbacher, O.D., FCOVD
Founder
Wow Vision Therapy
Get In Touch
Concerned you or your child may be struggling with a concussion-based vision problem and wish to learn more about vision therapy? Please fill out the form below and one of our Patient Care Coordinators will be in touch to answer your questions or help schedule an evaluation for you.
